You’re reading the web version of our email briefing on health policy, science and medical news. Sign up to get it next week.
Catching up this week on some stories you might’ve missed. Canada’s health system is under strain (we know this), and the people inside it are burning out.

If you’re a physician, there’s a good chance you’re depressed, according to a recent CMA survey of roughly 3,300 doctors.
42% screened positive for depression. That’s down from 48% in 2021 but still way up from pre-pandemic levels. Rates are highest among trainees entering the profession.
Alberta-based family physician Dr. David Keegan says more and more work is being downloaded onto primary care providers by governments, insurance companies and medical specialists. “People are feeling more like, I think, widgets in the machine.”
CMA President Dr. Margot Burnell says the profession is still carrying the pandemic’s weight, but in new forms: more complex patients, relentless paperwork, and a constant need to correct misinformation in the exam room.
She says team-based care (which would let doctors actually take time off) and digital systems that don’t force providers to chase data across half a dozen portals would help the situation.
Seven years ago, one in three doctors screened positive for depression and nearly one in five said they’d contemplated suicide. Many said they avoided seeking help out of shame or fear of professional consequences.
Burnell sees “hope at the end of the tunnel,” and says today’s physicians are a bit more willing to get help when needed.
Read more…

Ontario now requires international med school graduates to have attended an Ontario high school for at least two years to be eligible for competitive residency spots in the province.
The province says it’s “supporting Ontario-educated residents with international medical degrees” with the abrupt new policy. Critics say it’s discriminatory and will worsen the province’s doctor shortage.
The change blocks immigrant physicians from the first round of residency matching, when most of the spots are filled. Experts say it favours wealthy Canadians who studied medicine overseas. Ontario, where 2.5 million lack a family doctor, is the only province with this requirement. Fun Fact: StatCan expects the province’s population of over-65s to grow by nearly a million people over the next decade.
Read more…
New Brunswick’s plan to let pharmacists manage chronic conditions and strep testing promised to ease pressure on family doctors and ERs. It didn’t.
The pilot moved ahead after a Shoppers Drug Mart lobbyist pressed the province to expand pharmacists’ prescribing roles.
Six pharmacist care clinics opened in 2023, but pharmacists weren’t given the ability to order basic lab work. This meant pharmacy patients often had to go right back to their doctors, or to the ER. Warnings of “fragmented care” came true when overlapping services like N.B. Health Link and Maple (notably a part of Loblaw’s growing healthcare ecosystem along with Shoppers) added to the confusion. The province has since ended the pilot, finding no evidence it eased pressure on the health system.
Read more…

The College of Psychologists and Behaviour Analysts of Ontario (CPBAO), under pressure from the government to expand mental-healthcare capacity, voted to lower its training standards.
The regulator plans to nix its four-year work-experience rule for master’s graduates, recognize overseas credentials, and scrap the oral exam.
This will bring Ontario in-line with other provinces and pave the way for Ford-government changes that make cross-province licensing automatic. Health Minister Sylvia Jones’s office says it has “no plans” to legislate such changes, but at least two CPBAO Council members say this will increase risk to the public and that they’ve been pressured to go this route.
Read more…
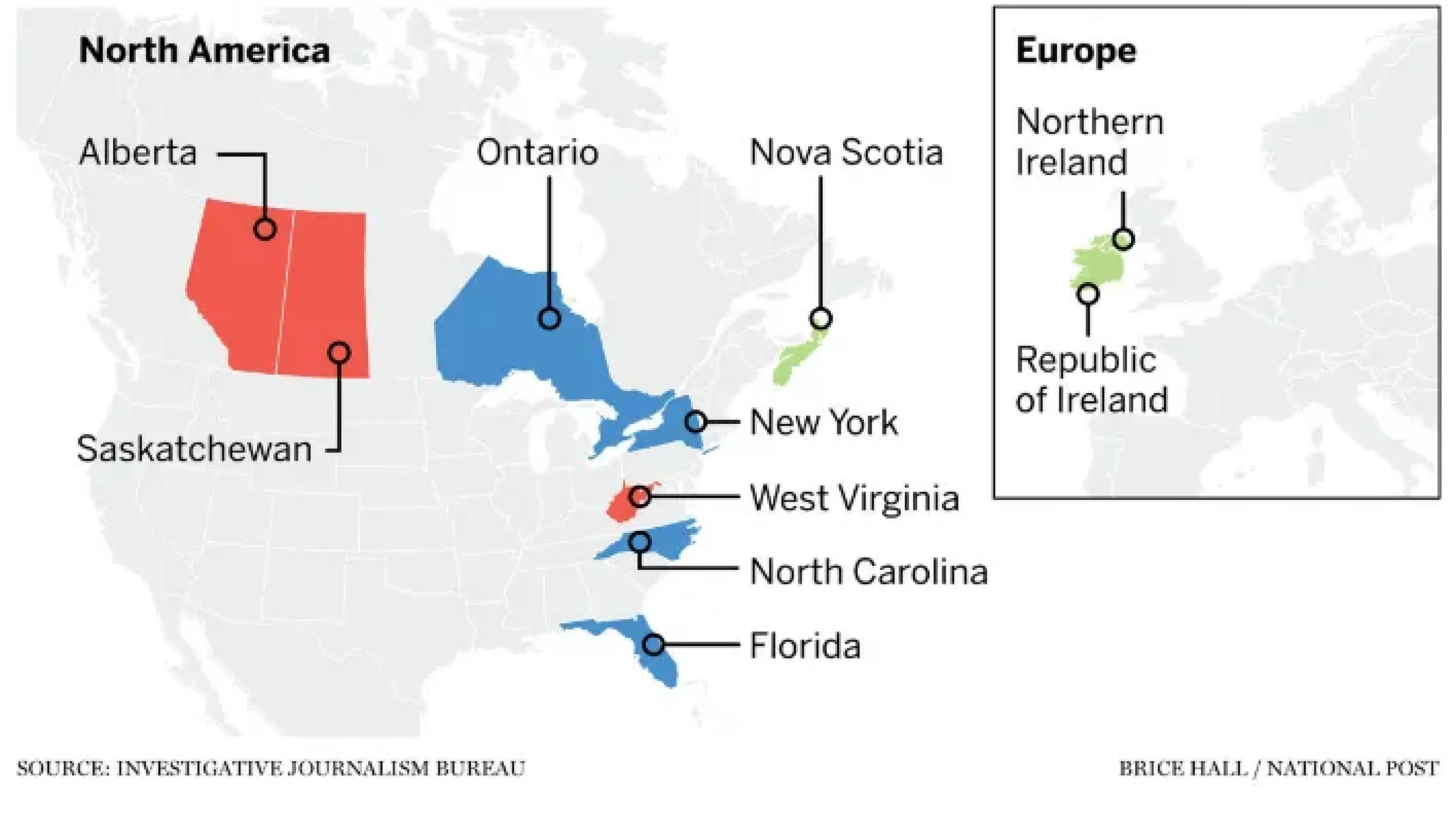
An international investigation has found more than 100 doctors disciplined or de-licensed in one place are now licensed and practicing elsewhere, including in Canada.
Physicians with histories of sexual misconduct and over-prescribing can easily get new licences after leaving other jurisdictions.
In Ontario, a doctor suspended over undisclosed prescription violations in multiple U.S. states now works without restrictions. In a system that leans heavily on self-reporting, the authors say their findings are “the tip of the iceberg.” As provinces work overtime to recruit international physicians, and pan-Canadian licensure looms ever-nearer, we may yet see a level of inter-provincial coordination that's long been lacking.
Read more…
That’s it for today.
If you made it this far, you probably care about this stuff as much as I do. Obviously, this makes you a very cool person.
Nick Tsergas, Editor
Canada Healthwatch
[email protected] | canadahealthwatch.ca
Stay informed.
On the most important developments in Canadian health.
Get Canada’s essential briefing on health policy, science, and system change. Get Briefing