You’re reading the web version of our email briefing on health policy, science and medical news. Sign up to get the next one.
Hi Healthwatchers 👩⚕️👨🏾⚕️👨⚕️👩🏻⚕️
H5N1 made more headlines than usual this week, and with good reason.
The U.S. response is looking, let’s say, less than pandemic-proof. Experts say we’re flirting with disaster. I’m saying this too, but experts are also saying it.
Elsewhere, Alberta turned its back on an easy fix for surgery delays, and family doctors are vanishing just when we need them most.

The U.S. is officially bungling this, letting the virus spread widely across hundreds of farms, with over 60 confirmed human cases, so far.
Why it's important: Despite billions spent to contain H5N1, the virus rages on due to failures in oversight, and short-term financial incentives at odds with stopping it.
Experts warn unanimously that the virus could mutate to spread between people, resulting in another pandemic. The more it spreads on farms, the more likely this becomes. California has declared a state of emergency, and a Louisiana patient is critically ill with the same strain that infected a B.C. teen. Early effects on food security are starting to be seen. Yesterday, H5N1 was detected on two Ontario poultry farms.
Read more…
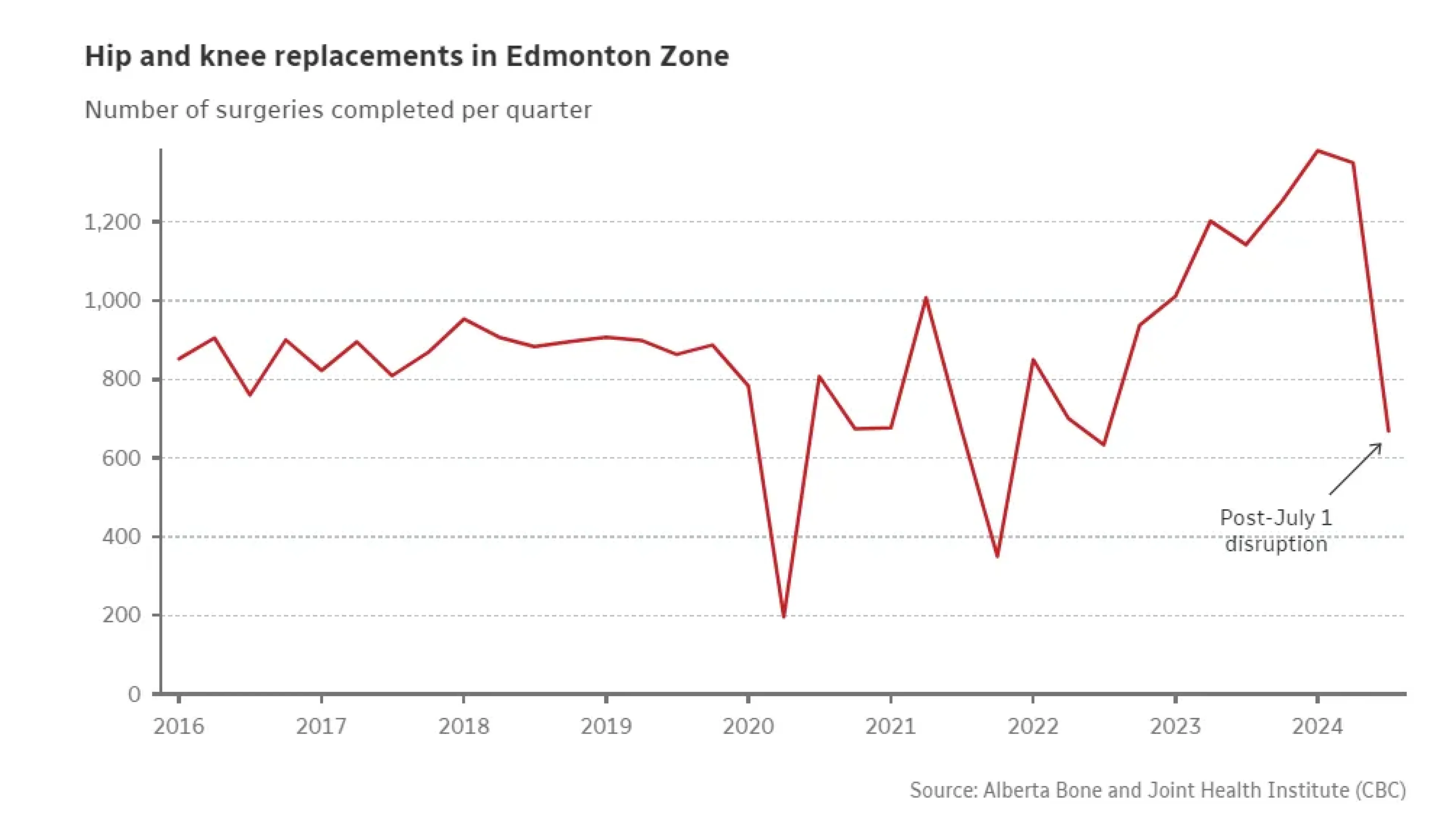
Alberta Health Services declined a $240,000 annual proposal to resolve a disruption in ortho surgeries at the Royal Alexandra Hospital, affecting roughly 2,500 patients yearly.
Why it's important: Doctors proposed funding hospitalists to provide overnight care, allowing in-patient surgeries to resume. AHS rejected the plan, insisting on “cost-neutral” solutions, despite half of Edmonton's joint replacements being postponed.
The disruption began when resident physicians, withdrawn due to accreditation risks, stopped providing overnight care. Surgeons declined to operate without adequate post-op support for medically complex patients. Experts say the plan’s cost is negligible compared to the human and economic toll of prolonged wait times.
Read more…

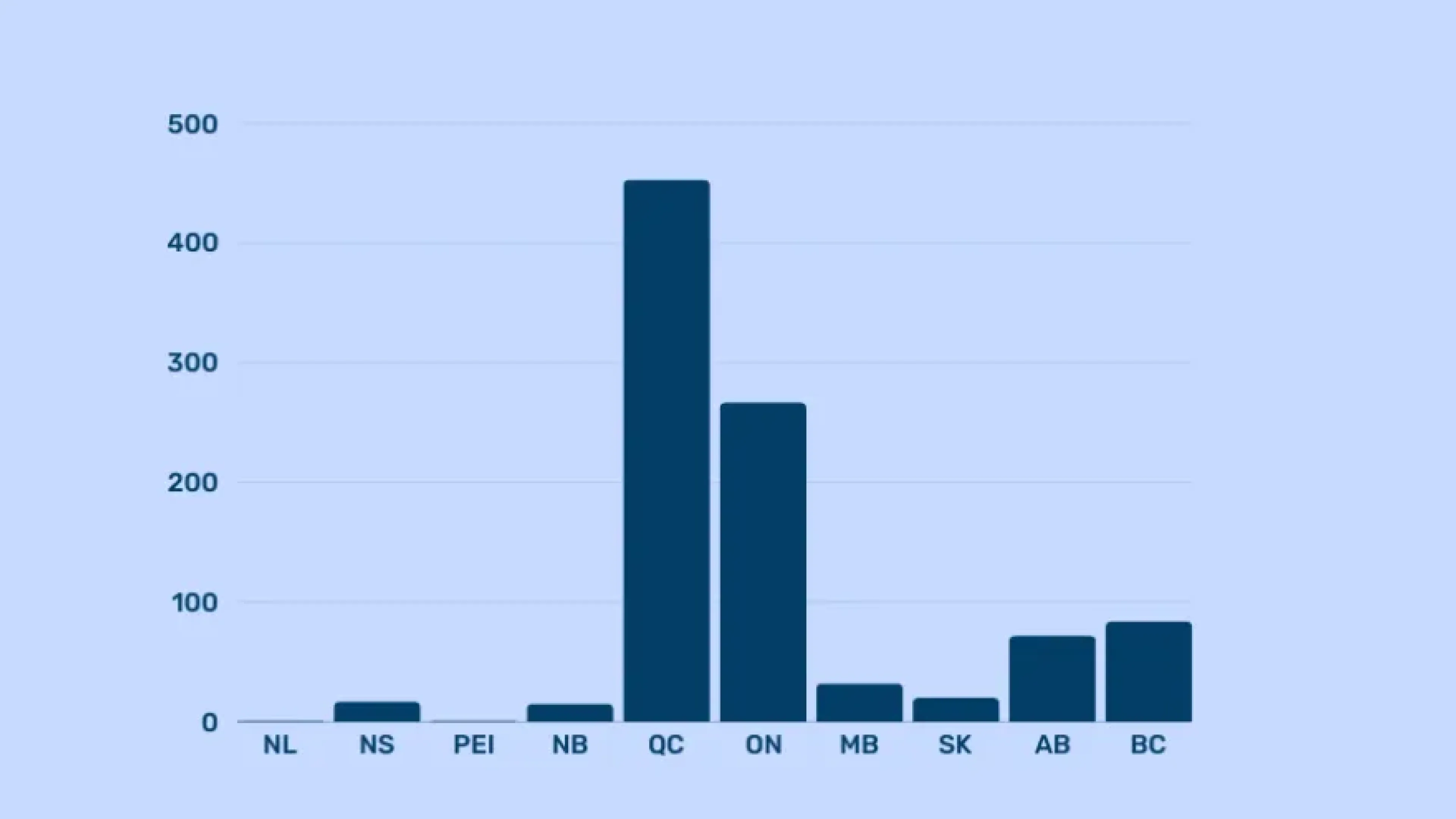
For the first time in roughly 30 years, Canada saw a decline in family physicians in 2023.
Why it's important: A new CIHI report shows Canada had 28 fewer doctors last year compared to the year before. It might seem minor, but it’s a nearly 3 per cent decline per capita, during a time of unprecedented population growth.
While numbers of nurse practitioners and pharmacists in primary care have grown, along with the things we’re asking them to do, family doctors are seeing fewer patients due to sicker populations requiring more time per visit. Administrative time for today’s complex patients is also markedly higher, and it’s no secret that family doctors are burnt out. What will it take to reverse the trend?
Read more…

Provinces and municipalities are getting creative in the quest to recruit doctors.
Why it's important: Doctor shortages are a significant driver of surgical waits and rural ER closures. Three solutions popped up this week.
Alberta’s new pay model incentivizes family doctors to take on more patients and provide after-hours care. Positive step, though effects on care access and ER pressure will take time to be felt. Manitoba is luring U.S. doctors with ads spotlighting universal healthcare and a (relatively) favourable political climate, and Colwood, B.C. is hiring on doctors as city employees, offering salaries, pensions, and paid vacations, a Canadian first. Doctors I’ve heard from on this last one are interested.
Read more…

Ontario hospitals and long-term care homes spent nearly $1 billion on temporary staffing last year, paying double or triple standard wages. New legislation will compel agencies to disclose their rates to the Health Minister.
Why it's important: Unregulated agency fees inflate system costs and strain health budgets. The move should help curb price gouging in the medium to long-term.
Health Minister Sylvia Jones calls the measure a step toward monitoring agency practices, though critics say it lacks immediate impact and teeth. "It will allow us to more easily measure and see whether we are seeing stabilization, increasing use, decreasing use, and where," Jones said. Whether the initiative evolves into robust reform remains to be seen. With more data, the potential is there.
Read more…
Gambling-related suicides occur roughly every nine days in Canada, with at least 963 deaths linked to gambling addiction since 2000.
Why it's important: A U.S. study strongly linked state legalization of sports betting to rising rates of domestic violence. Despite known risks, some provinces are making gambling more frictionless and available.
John Hallett’s story illustrates the human cost. After his wife’s death, the retired factory worker lost $380,000 at the casino, eventually losing his home and ending his life. Inconsistent provincial data and no national standards lead to large gaps in tracking gambling-related suicides. Experts estimate up to 10 per cent of suicides are actually gambling-related.
Read more…
And with that, we conclude this Weekly Dose.
I’ll be taking a break on newsletters for the next two weeks, but will be back on Jan. 12 with a new edition. Healthwatch, though, never stops and will keep chugging along over the holidays.
Wishing you all a relaxing holiday and healthy 2025. ✨
See you next year,
Nick Tsergas, Editor
Canada Healthwatch
[email protected] | canadahealthwatch.ca
Stay informed.
On the most important developments in Canadian health.
Get Canada’s essential briefing on health policy, science, and system change. Get Briefing