You’re reading the web version of The Weekly Dose, our newsletter on Canadian health care and medical news. Sign up to get it next week.
Welcome Healthwatchers! 👋
Today—on World Health Day—we're tackling some tough questions that are really shaping our healthcare universe. It’s been a packed week of policy, controversy, and real-world impacts that certainly got me thinking.
Does Canada need a Primary Care Act?
In a recent op-ed (and prelude to her book launch) former federal health minister Jane Philpott advocates for the right of every Canadian to have a family doctor.
Why it's important: Pointing to the patchwork nature of Canadian healthcare—and the millions of people without access to primary care—Philpott argues for a systematic, national approach to primary care, akin to the universal access model of public schooling.
Philpott’s proposed Act would assign every Canadian to a "primary-care home" based on their location, improving access and continuity of care. Drawing parallels with successful systems in New Zealand, Norway and elsewhere, she argues that primary care-focused systems not only deliver better patient outcomes, they’re also cost-effective. Philpott's book, which outlines her policy prescriptions for our healthcare woes, is set to launch this week, on the 40th anniversary of the Canada Health Act.
Read more (Pre-order the book)
Rising alert on H5N1: what you should know
H5N1 Avian Flu is making headlines as it infiltrates dairy herds across six U.S. states, jumping from birds to mammals, and in rare cases, people. With a case fatality rate of 52% among known human infections, it far surpasses the mortality rates of COVID and seasonal flu.
Why it's important: Epidemiologist Raywat Deonandan wrote us a fantastic summary of where things stand right now. With media attention spiking, it's a valuable and succinct read for anyone following the story.
Canada's experience with H5N1 has thus far been limited to a single fatal case believed to be linked to travel—this was 10 years ago. Today, the likelihood of the virus adapting for human transmission seems to be on the rise, raising legitimate fears of a new pandemic. Despite this, experts emphasize that H5N1's spread can be managed with existing vaccines and stringent food handling. In his piece, Deonandan offers key insights, and calls for strategic focus on preparedness rather than fear.
Read more…
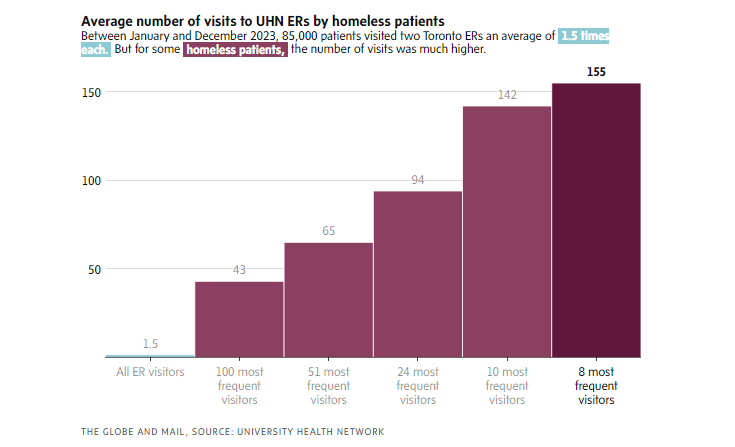
Is housing the solution to Canada's ER crisis?
The challenge of frequent ER visits by homeless individuals has prompted hospitals to adopt new strategies. Royal Alexandra in Edmonton provides transitional housing to patients otherwise facing discharge into homelessness. The program has reduced ER visits and put participants on paths to permanent housing.
Why it's important: This housing-first approach offers a more compassionate alternative to what we’re currently doing, while addressing the underlying social determinants of health.
As ERs become last resorts for growing numbers of unhoused people, the urgency of systemic change is undeniable. Toronto's UHN is also setting a precedent with a housing complex integrated with health services, aiming to relieve pressure on ERs and improve outcomes. These pioneering programs blur the line between health and housing, challenging the separation of these sectors and embodying what it really means to have a holistic approach to healthcare. Hospitals in every major city will want to watch data from these programs closely.
Read more…
Nova Scotia wants to get Physician Assistants into Primary Care
N.S. Health is pioneering a shift to integrate physician assistants (PAs) into primary care. The initiative is the latest option on a growing menu of fixes to provinces’ ailing primary care systems.
Why it's important: With many family doctors approaching retirement, the incorporation of PAs could significantly mitigate the province's looming primary care crunch.
Working under the supervision of physicians, PAs can handle straightforward cases, assist in surgeries, and prescribe medications, thereby enhancing the efficiency and accessibility of healthcare services. The program, which began with a pilot in 2019, has seen PAs make notable contributions in various medical departments. Although the approach shows promise, it is sure to ignite familiar discussions around scope overlap between roles, regulatory and licensing challenges, the quality and depth of PA training, and ultimately, how patients perceive and accept care from PAs. N.S. Health officials are currently planning a recruitment effort in the U.S. for later this year.
Read more…
Funding flows to for-profit LTC companies facing class action lawsuits
Despite facing class-action lawsuits, six Ontario long-term-care operators are set to receive billions in government funding.
By the numbers:
- 200: Facilities owned or operated by sued corporations.
- 78%: Portion of recent funding expansion funding for for-profit LTC facilities, specifically awarded to companies involved in gross negligence lawsuits.
- 31,000: New LTC beds promised by Ontario by 2028.
- 28,000: Existing beds to be refurbished by 2028.
- 1,228: Net new beds added to Ontario's long-term care system as of March 2023.
- 44,000: People wait-listed for LTC beds in Ontario as of December 2023.
- 57%: Market share of long-term care in Ontario provided by for-profit corporations in 2021, the largest in Canada.
The ongoing legal actions juxtaposed with the multibillion funding expansion really do show a need for transparency and oversight in the allocation of public funds. The cases raise questions about the adequacy of care provided by the companies named in the suits, and also around the deeper implications of private equity’s growing involvement in our long term care.
Read more…
Hamilton mayor Andrea Horwath pushes back on plan for paid plasma donations
Andrea Horwath wants to block a Spanish company from opening a blood plasma collection clinic in Hamilton, declaring the city a "paid-plasma-free zone," In a Spectator interview she said, "anything that preys upon the most vulnerable is hideous and doesn’t belong in Hamilton.”
Why it's important: Regular readers will know I’ve been following this one closely, and this development comes as a bit of a surprise. Horwath’s motion (pending a city council vote), challenges both Canadian Blood Services' (CBS) exemption from Ontario's Voluntary Blood Donations Act and the broader ethics of compensating plasma donors.
Horwath's stance and comments reflect deeper contentions with the growing trend of paying blood donors for their plasma. The discussion is resurrecting old questions around the ethics of blood donation, reminiscent of both the tainted blood scandal of the ‘80s and Horwath’s staunch opposition to paid donation clinics a decade ago during her tenure as both Hamilton MPP and leader of the Ontario NDP. As awareness of these clinics grows provincewide, Mayor Horwath has set a precedent for municipal involvement in the inevitable public debate, and once again positioned herself at odds with the provincial government, which has greenlit CBS’ plan.
Read more…
And that's it for this edition. 🙂
I’ll be back next week with a new slate of topics to dissect. On this World Health Day, I'm grateful for people like you, who are demonstrably committed to staying informed and pushing for systems that truly serve us all. Thanks for tuning in.
Yours in health,
Nick Tsergas
National Health News Editor
Canada Healthwatch
[email protected] | canadahealthwatch.ca