West Nile virus season returns — a medical epidemiologist explains how it’s transmitted and how you can avoid it
West Nile virus is the most common mosquito-borne illness in the continental U.S., with an average of 2,464 reported cases per year.
Every August, West Nile season ramps up, primarily in parts of the Southern and Western United States.
The Conversation U.S. asked neurologist and medical epidemiologist Daniel Pastula to explain what researchers know about West Nile and how to protect yourself from contracting the disease.
What is West Nile virus?
West Nile is a virus that was first identified in the West Nile region of Uganda in 1937 and subsequently caused outbreaks throughout Africa, the Mediterranean region and parts of Europe.
It arrived in the New York City area in late 1999, probably from an infected bird or mosquito. The virus has since spread and become endemic throughout the continental United States and other parts of North America.
How is West Nile virus transmitted?
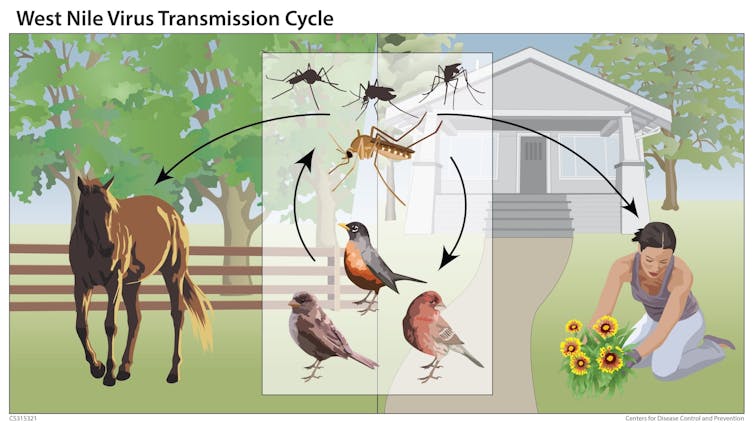
West Nile virus is primarily transmitted to humans by mosquito bites. West Nile virus exists in a transmission cycle between various birds such as crows, robins and blue jays and primarily several Culex species of mosquitoes, which are very common across the U.S.
The mosquitoes become infected by feeding on infected birds with high levels of virus. Then the infected mosquitoes pass the virus to other birds by feeding on them.
Sometimes, an infected mosquito will bite a human, horse or other mammal, transmitting the virus to them. However, these animals do not develop a high enough viral level in their blood to keep the cycle going. In other words, they are “dead-end” hosts.
Rarely, West Nile virus is transmitted in other ways, including through accidental laboratory exposures, blood transfusion or organ transplantation. Very rarely, it may be transmitted during pregnancy, delivery or through breastfeeding.
When and where does it show up, and is it seasonal?
In the continental U.S., most human cases of West Nile virus disease occur from July through September, or until the first hard freeze or snowfall. This is commonly called “West Nile season.” By this time of year, mosquitoes have had enough time to emerge, feed on infected birds and become infected themselves.
In more southern areas such as Arizona, Florida and Texas, mosquito transmission may occur earlier than July and later than September. For example, mosquitoes infected with West Nile virus were reported in Texas as early as May 2024.
While human cases of West Nile virus disease have occurred in the 48 continental states, the District of Columbia and Puerto Rico, the majority of cases over the past two decades have been in the Great Plains, Southern and Southwestern United States. This likely has to do with the types of mosquitoes, birds, bird migration patterns, temperature, rainfall and irrigation practices in these areas.
How dangerous is West Nile?
Approximately 80% of people infected with West Nile virus have no symptoms or very mild ones.
But about 20% of the time, people infected with West Nile virus can develop a sudden flu-like illness with symptoms such as high fever, headache, muscle and joint aches, stomach problems such as nausea, vomiting and diarrhea, rash and fatigue within two to 14 days after being bitten by a West Nile-carrying mosquito.
Most people recover from this “West Nile fever,” but the fatigue may last weeks to months.
In about 1% of cases, however, the virus can invade the covering of the brain, causing what is called meningitis; the brain itself, resulting in encephalitis; or the spinal cord, causing a polio-like syndrome. When the virus invades the nervous system like this, it is called “West Nile neuroinvasive disease.”
Approximately 10% of West Nile neuroinvasive disease cases are fatal, particularly in cases where the brain and spinal cord are directly infected. Many survivors are left with permanent neurological disability such as weakness, movement disorders or cognitive issues to varying degrees.
The risk of West Nile neuroinvasive disease is higher in people who are 60 or older, those who are immunocompromised and those with conditions such as cancer, diabetes or kidney failure.
Are there any treatments or vaccines?
While a variety of treatments have been investigated, there are currently no proven antiviral treatments for West Nile virus disease. Treatment remains largely focused on addressing symptoms.
Some patients may require over-the-counter medications for fever and headaches, fluids for dehydration, anti-nausea medications for nausea or vomiting, and rest. Some may require hospitalization and treatment for severe dehydration, organ dysfunction, seizures or brain swelling.
There are currently no West Nile vaccines licensed for use in humans, though some vaccine candidates and ideas are being studied.
How can you help prevent it?
Generally speaking, if you prevent mosquito bites, you prevent West Nile virus infection. There are several things you can do to prevent mosquito bites:
First of all, use an Environmental Protection Agency-registered insect repellent on exposed skin when you are outside in an area with mosquitoes. These are safe and effective when used as directed.
You can also wear long-sleeved shirts and pants when feasible. It is much harder – or even impossible, depending on the fabric – for mosquitoes to bite through clothing. You can also treat your clothing with permethrin, an insecticide, which further repels mosquitoes.
When possible, avoid being outside between dusk and dawn. This is when the West Nile-carrying mosquitoes are most active.
It’s also a good idea to get rid of any unneeded standing water in places such as birdbaths or kiddie pools around your property, as mosquitoes like to breed in standing water. When indoors, be sure that any unscreened windows are closed to keep mosquitoes outside. These simple precautions can greatly reduce the risk of getting severely ill.
In addition to these precautions for individuals, robust public health and vector control programs help to monitor and control the spread of West Nile virus by warning area residents of the presence of the virus and reducing infected mosquito populations when necessary.![]()
Daniel Pastula, Professor of Neurology, Medicine (Infectious Diseases), and Epidemiology, University of Colorado Anschutz Medical Campus
This article is republished from The Conversation under a Creative Commons license. Read the original article.