‘Morning Healthwatchers! 👨🏻⚕️
Today's issue brings a mixed bag of topics: some disheartening, some promising, and more that honestly were a bit emotional to write about. From barriers faced by undocumented migrants to innovative mental health treatments that could change lives. Let’s see the news.
Canada's pharmacy regulators signal crackdown on insurer–pharmacy exclusivity deals
Several provincial pharmacy regulators are evaluating measures to limit exclusivity agreements between insurers and pharmacies.
Why it's important: If enacted, regulations would aim to preserve patient autonomy in choosing their healthcare providers, in an effort to address concerns over the influence of big business on the pharmacy sector.
Regulators across Canada are responding to the controversy over preferred pharmacy networks (PPNs) which require patients to buy certain medications from specific pharmacies. The practice gained notoriety when Manulife attempted to establish a PPN with Shoppers Drug Mart, prompting backlash and ultimately, the deal’s cancellation. The Ontario College of Pharmacists proposed guidelines to discourage PPNs, taking inspiration from Quebec. Most provincial pharmacy regulators are now considering similar measures.
Read more…
An undocumented woman was denied an emergency C-section at an Edmonton hospital
Perla Estrada was reportedly denied an emergency C-section at Royal Alexandra Hospital unless she paid them $5,000 upfront.
Why it's important: This is shedding some light on the daunting healthcare barriers undocumented migrants encounter and the at-times dystopic realities they face, especially in emergencies.
Estrada was told she needed an urgent C-section due to low amniotic fluid but says she was denied the procedure until she coughed up $5K. Fortunately, she was able to have her C-section done at another hospital. Alberta Health Services is investigating, as their policy ensures emergency care regardless of financial status, but the story raises important questions about the treatment of undocumented immigrants in health settings and the policies that both hospitals and provinces have in place to make sure care isn’t withheld in life-threatening situations.
Read more…
BC to address illicit drug use in hospitals with new provincial policy
Responding to complaints from nurses, as well as significant media attention, the B.C. government plans to implement a standardized provincial policy on illicit drug use in hospitals.
Why it's important: In a particularly illustrative example of the problem’s scope, nurses reported substance use on a perinatal unit, intensifying calls for change.
The government’s new initiative seeks to create "designated spaces" for drug use on or around hospital grounds. This follows a report pointing to failures of current protocols to protect workers from occupational drug exposure risks via inhalation. The proposed policy will unify the rules across all B.C. hospitals. The nurses’ union says the problem has always been a background issue, but that it’s ramped up in the last year since B.C.’s drug decriminalization pilot project began. What’s not clear about the new policy is what mechanisms will be put in place to enforce it.
Read more…
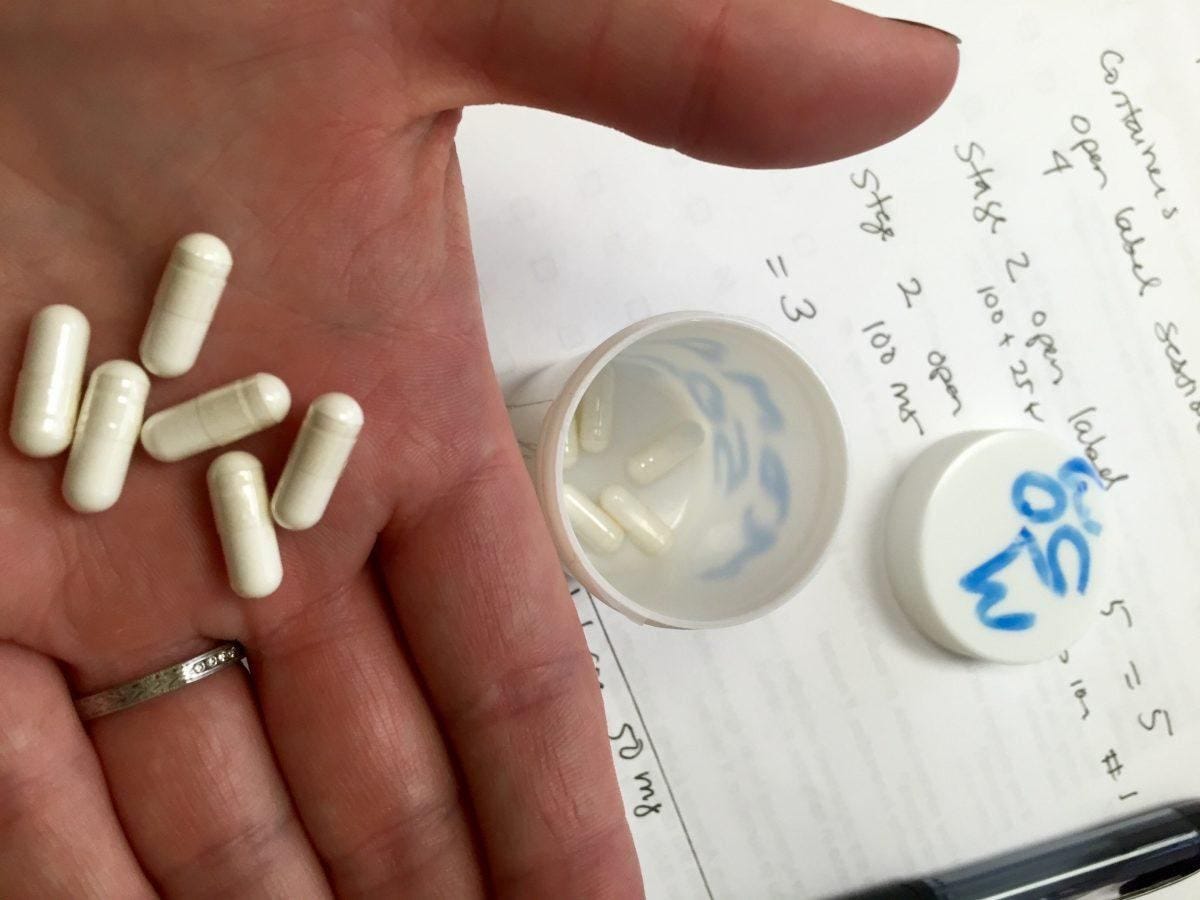
Psychedelics poised for pharmaceutical approval as mental health treatments
80 years after the first accidental LSD trip, psychedelics are advancing in medical fields, with FDA approvals on the horizon for treating mental health disorders.
Why it's important: If this happens, it could legitimately revolutionize treatment options for anxiety, depression, and PTSD—which haven’t changed much in 20 years—offering people relief that has been shown to be both rapid and durable.
Recently, the FDA granted breakthrough designations to two Canadian companies working on these compounds, enabling a faster review process due to promising early results. These drugs have shown potential to significantly improve symptoms of anxiety and depression with just a single dose. Historically stigmatized and regulated under strict drug laws, recent studies have re-evaluated their therapeutic potential, leading to a resurgence of interest from both the scientific community and investors. Read more…
What to know about Arizona’s near-total 1864 abortion ban
Arizona is poised to enforce a near-total abortion ban from 1864, drawing significant legal and political attention.
Why it's important: The archaic law, complete with strict prohibitions and severe penalties, places Arizona at the forefront of national (and international) debates on reproductive rights.
The Arizona Supreme Court has cleared the way to enforce a Civil War-era law that bans nearly all abortions, nominally allowing exceptions to save a mother's life, though in other states with abortion bans, women have had difficulty accessing care under such ‘exceptional circumstances.’ The decision dismisses the allowance of abortions within the first 15 weeks of pregnancy. Enforcement of the law could lead to severe implications for healthcare providers, with potential prison sentences for those found performing abortions outside the narrow exceptions (ostensibly) allowed.
Read more…
Tragic end for quadriplegic man raises questions over healthcare negligence

After a preventable bedsore led to severe suffering and a bleak prognosis, Normand Meunier opted for medically assisted death.
Why it's important: Meunier’s story is garnering significant public attention. His case exemplifies the dire consequences of health system shortcomings, and may spur some policy action in Quebec.
Meunier opted for MAiD after a severe bedsore developed during a four-day stay on an ER stretcher. Despite requiring an alternating pressure mattress to prevent such injuries, he was left on a stretcher without proper care, leading to his devastating condition. Meunier’s widow, Sylvie Brosseau, argues that the incident was a failure by the hospital to provide basic care, and is calling for an inquiry into Quebec’s handling of similar cases. The story has sparked intense debate about both the adequacy of emergency care and the ethics of MAiD as a last resort for those failed by the system.
Read more…
And on this pensive note, we’re all done today.
These stories, while they may challenge us and make us feel things, are important. They remind us why we must continue to advocate for improvements and stay informed about the developments that impact us all. I hope today’s issue provokes thought, spurs conversation, and inspires you.
Thanks for being here,
Nick Tsergas
National Health News Editor
Canada Healthwatch
[email protected] | canadahealthwatch.ca