You’re reading the web version of The Weekly Dose, our newsletter on Canadian health care and medical news. Sign up to get it next week.
Good morning, and welcome to your Weekly Dose.
This week, a veritable buffet of delicious health stories, all of them very much “of the moment.” From mycoplasma’s moment in the sun to the latest on national pharmacare (apparently it isn’t dead), these are the stories that stuck out to me this week. Read on for the breakdowns and hopefully, some helpful insights from me. Enjoy!
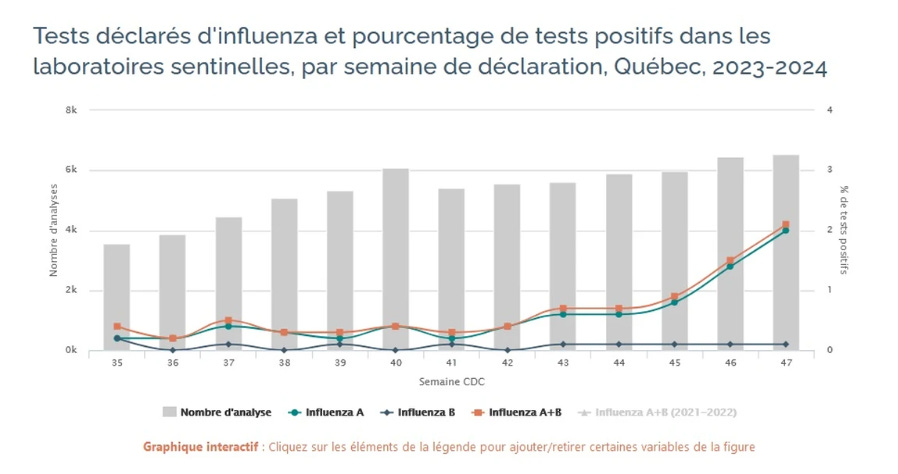
Quebec monitoring for mycoplasma pneumonia in kids
With Mycoplasma pneumoniae on the rise globally, Quebec health authorities are vigilant. While local cases haven't yet spiked, experts are monitoring.
Why it's important: Adding a layer of mycoplasma cases on top of last year’s mix of tripledemic pathogens is concerning for our stretched health systems, as well as the potential for emerging antibiotic resistance.
Initially reported in China, with subsequent epidemics in France, Denmark, the U.S., South Korea, Ireland, and the Netherlands. Mycoplasma is by no means a new pathogen. Currently, it's notable that mycoplasma is causing illness and hospitalization at higher volumes than what's typically observed. A possibility we should consider is that Canadian hospitals may already be dealing with an uptick in mycoplamsa pneumonia, but not testing for it. Hospitals are facing very high occupancy, compounded by nursing shortages and the onset of flu season. With RSV kicking off, and COVID still doing its thing, our healthcare systems brace for further impact.
Read more…
Canada's drug shortages prompt growing concern
Canada faces over 1,800 drug shortages. Experts point to global manufacturing issues and limited domestic production as key factors.
Why it's important: These shortages pose significant health risks, especially for people dependent on specific medications for chronic conditions.
The shortages are attributed to factors such as global manufacturing consolidation and reliance on overseas production. Significant proportions of pharmaceuticals and their ingredients are produced in China and India, creating vulnerability in Canada's drug supply. The impact of the shortages is profound, causing stress and health risks for patients unable to access critical medications. There is an additional burden placed on healthcare providers, with pharmacy teams spending considerable time managing shortages. Solutions such as expanding pharmacists' prescribing powers and onshoring manufacturing are being floated. Health Canada's drug shortages unit is working on sourcing imports from a broader range of countries, aiming to build a more resilient drug supply.
Read more…
Pharmacare negotiations remain cordial amidst political pressures
Discussions on pharmacare legislation continue, with a focus on achieving universal coverage, despite missing the 2023 deadline.
Why it's important: The legislation, if enacted, will significantly impact healthcare accessibility and affordability for Canadians.
Despite a supply-and-confidence agreement hinging on the passage of the Canada Pharmacare Act by the end of 2023, both parties seem agreeable to extending the deadline, to ‘get the legislation right.’ The NDP emphasize that they remain firm on the need for universal coverage, having rejected the Liberals' initial proposal. The fiscal implications and political dynamics, including pressures from the NDP's base and the Liberal government's current economic woes, add layers of complexity. Despite the challenges, Health Minister Mark Holland called the discussions “fruitful and positive.”
Read more…
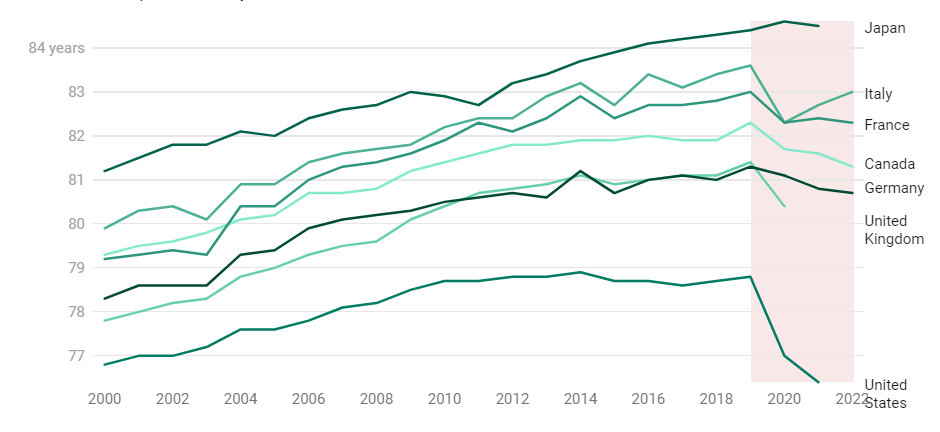
Young Canadians’ deaths are behind the drop in life expectancy
Life expectancy in Canada fell to 81.3 years in 2022, largely due to COVID and the opioid crisis disproportionately affecting death statistics in younger demographics.
Why it's important: This decline reflects significant public health challenges, namely the ongoing opioid crisis as well as COVID, which saw its death toll rise in 2022.
Nearly 20,000 Canadians succumbed to COVID last year, making it the third-most common cause of death in the country. Concurrently, increases in opioid deaths were particularly pronounced in men aged 30-45 and women aged 25-35. The global context reveals a related trend, with most G7 countries experiencing similar drops in life expectancy since 2019—so it’s far from just a Canadian phenomenon. Despite expected declines in COVID-related deaths, both issues will continue to impact our public health outcomes for years.
Read more…
Saskatchewan outsources cancer screenings to a private clinic in Calgary
In response to staff shortages and a lengthy waitlist, Saskatchewan is sending breast cancer patients to a private clinic in Calgary for imaging.
Why it's important: The decision shines a spotlight squarely on the province's struggle with medical staff retention and health system capacity.
While this measure provides immediate relief to patients facing long wait times, and is necessary as a stopgap to avert significant morbidity and mortality, it raises serious concerns about the sustainability of Saskatchewan's healthcare infrastructure. The underlying staff shortages driving the imaging waitlist’s growth point to an urgent need to address working conditions and competitive pay to retain health professionals. This outsourcing strategy, though practical in the near-term, indicates a reactive rather than proactive approach to health system management, and it highlights the need for long-term planning to improve the provincial health system's resilience and self-sufficiency.
Read more…
A family doctor in Ottawa is facing deportation, sparking immigration policy debate
Dr. Carmen Bilcea, a family practitioner currently serving 1,200 patients in Ottawa, had her permanent residency application denied due to her age and marital status, among other criteria.
Why it's important: The case highlights the escalating societal tension between immigration policies and healthcare staffing needs in Canada.
The denial of Dr. Bilcea’s permanent residency not only disrupts her life, it will ripple across the lives of her 1,200 patients and their families—and her colleagues—amidst a severe and worsening family doctor shortage. The situation illustrates the challenges within Canada's immigration system, particularly for health professionals. With over two million Ontarians without a family doctor, and that number set to double within the next five years, the case raises critical questions about the alignment of our immigration policy with the country’s urgent health needs. With anti-immigration sentiment now on a sharp upswing, I’d speculate that hyper-targeted policy approaches to retaining these workers will become more attractive to governments.
Read more…
Thanks so much for joining me in another edition of the Weekly Dose. As our platform continues to mature, I’m very excited to announce that we’ll soon be rolling out a Featured Ink section on Canada Healthwatch. If you're reading this, chances are pretty good you have an health issue that’s near and dear to you. Honestly I’m pretty tickled (and humbled) when I look through the list of brilliant folks who are reading this week to week. If you have something you’d like to write about, I invite you to get in touch with me ([email protected]) so we can chat about it.
Yours in health,
Nick Tsergas
National Health News Editor
Canada Healthwatch
[email protected] | canadahealthwatch.ca